© VIB
Thanks to advanced single-cell technology, a team of researchers under the supervision of medical oncologist prof. dr. Oliver Bechter (UZ Leuven) and prof. Jean-Christophe Marine (VIB-KU Leuven Centrum voor Kankerbiologie) was able to discover a specific group of cancer cells that induce resistance to immunotherapy. As a result the team was able to develop a strategy to get rid of these cells and to significantly increase the efficacy of immunotherapy in preclinical models. The results of the study were published in Cell.
In-depth dissection of the tumour ecosystem.
Immunotherapy, a treatment that uses the patient's own immune system to fight tumours, has emerged as a pioneering method of cancer treatment. Recent developments in this area have shown promising results, especially for patients with advanced skin cancers such as melanoma. However, the method is not without its challenges. Less than 50% of melanoma patients react well to immunotherapy. The underlying reason for therapy resistance is not yet completely clear at this point in time.
This prompted the team of researchers to make use of new technologies that allow in-depth dissection of the tumour ecosystem at an unprecedented level of detail. This achievement was supported by the VIB Grand Challenges Programma and was executed in collaboration with prof. dr. Oliver Bechter and prof. dr. Francesca Bosisio from UZ Leuven. The objective of the research was to discover the underlying factors that contribute to immunotherapy resistance.
Mapping melanoma tumours
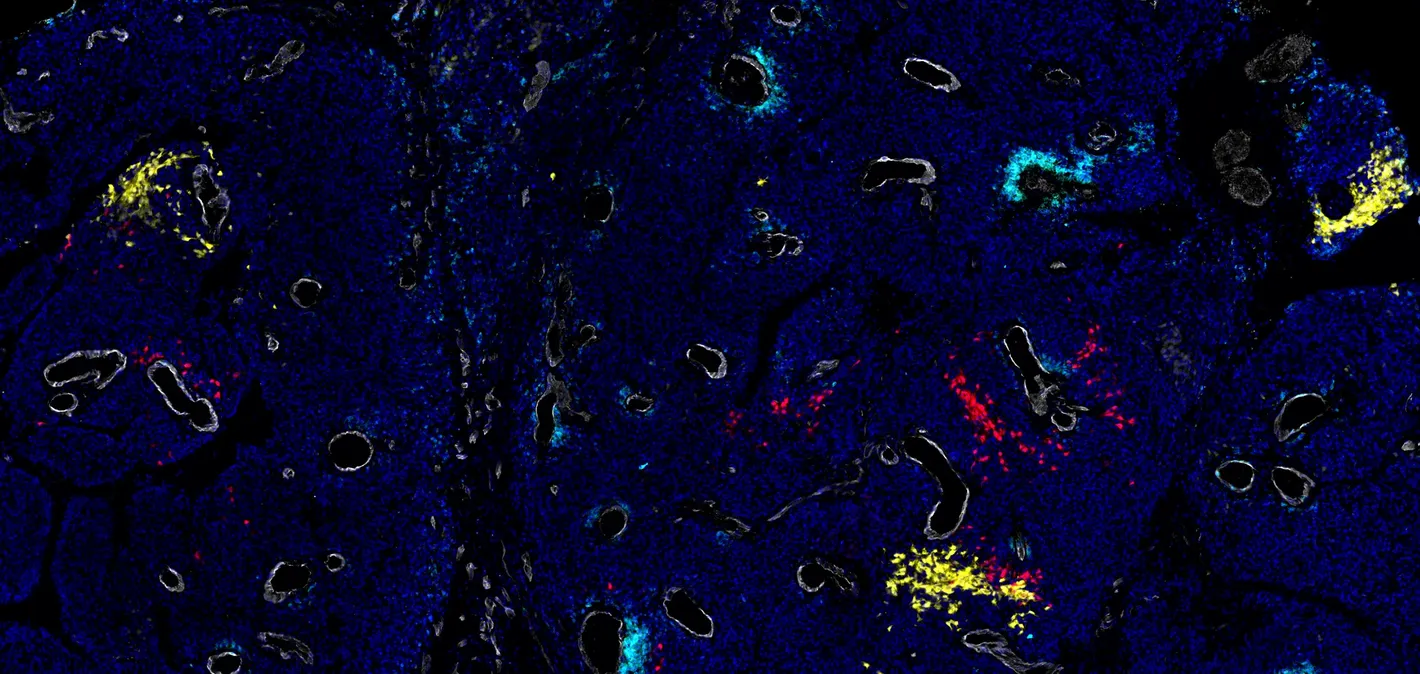
In a first step the research team thoroughly analysed every cancer cell in melanoma lesions of more than 20 patients. With the help of advanced single-cell technology and spatial technologies they were able to successfully characterise every individual cancer cell and mapped their precise location within the complicated architecture of the tumour.
Dr. Ewout Landeloos (Marine Lab), Joanna Pozniak (Marine Lab) and Dennis Pedri (Marine/Annaert Lab), co-first authors of the research paper: "Thanks to a close collaboration with UZ Leuven we were able to use samples from melanoma patients undergoing an immune checkpoint blockade (ICB) treatment and examine these for a longer period. This is the standard treatment for most melanoma patients. Very specifically, we collected biopsies from patients both before the start of treatment and 3 weeks after. Through data analysis of single-cell RNA sequencing, we obtained detailed insights into the cellular composition of melanoma lesions and their behaviour during treatment."
The team generated a blueprint for every tumour in high resolution. Their findings showed that melanoma consist of a diverse range of cancer cells, each showing its own characteristics. More specifically, the unique characteristics of each cell appeared to be influenced by their location withing the tumour and by the way the cell communicates with neighbouring cells.
From A to B
With a detailed map of melanoma tumours at hand, the researchers try to identify the cell types that were associated with immune therapy resistence. Surprisingly, the so-called mesenchymal-like cell types, a subtype that looks like stem cells, appeared both rare and indicative for reduced immune response. The team concluded that those mesenchymal-like melanoma cells have an remarkable ability to hide from immune attacks and potentially facilitating an environment that compromises immune system activity. As a result they contribute to treatment resistence.
The team then discovered that the mesenchymal melanoma cell's ability to hide depends on a gene named TCF4. In addition to previous research that identified a therapeutic strategy that efficiently targets this specific molecule, the team showed that this approach can be used to to sensitise refractory melanomas to ICB in preclinical models.
By blocking certain tumour cells in experimental models, the response to immunotherapy could be repaired, which suggests that we have identified a new treatment target in melanoma patients that justifies further clinical research.
Prof. dr. Oliver Bechter: "The clinical study, executed at UZ Leuven, was a biomarker study specifically designed for this Grand Challenge project. Tumour samples were collected from melanoma patients right before and after the first cycle of immunotherapy. By applying the advanced technology in single cell analysis, we were able to identify early changes in the tumour that predicted whether patients would react to the treatment. Additional experiments revelead that a specific tumour cell type was responsible for the failure of the treatment. By blocking these tumour cells in experimental models, the response to immune therapy could be restored, which suggests that we have identified a new treatment target in melamona patients that justifies further clinical research."
The findings of this research suggest that re-using an epigenetic drug (such as BET blockers) to target the TCF4 gene can be a may be a viable solution to improve immunotherapy success in patients. More research and clinical studies will be necessary to validate these findings and assess the efficiency of the proposed treatment strategy.
The research described was made possible thanks to the generosity and courage of the melanoma patients that participated in this study, as well as thanks to the VIB Grand Challenges Programme, FWO, the Marie-Sklodowska-Curie fonds and Stichting tegen Kanker.
More info about the VIB Grand Challenges Programme on https://vib.be/nl/research-and-impact/grand-challenges